Intra-uterine contraceptive devices (IUD) types complications and contra indications of IUD use
One of the main contraceptive methods in use worldwide. It is the insertion of inert material inside the uterus in order not to allow pregnancy to happen. . .
HISTORY
In 1909_Ralph Richter from Germany showed the efficacy of mechanical contraception by inserting silk warm gut suture in the endometrial cavity.
Between 1928_1930 Granfenberg from Berlin presented three reports on silk star devices, and he is known as the pioneer of the IUD.
The Ohta ring was used by Ishehama from Japan. The ring was first made of gold and later from plastic.
In early 1960s Lippes loop and Margolines spiral made of biologically inert polyethylene appeared.
In 1970s hormone-releasing IUDs developed but their real use started in 1995.


TYPES OF Intra uterine contraceptive devices
1. Medicated IUD:
Those IUDs that carry biologically active agents into the uterine cavity like levonorgestrel-releasing device [MIRENA]. It is an intrauterine system (LNG_IUS) that has sleeves of levenorgestril 52mg around its stem releasing 20 microgram/day and lasting for at least five years. The advantage of medicated IUDs is that the carrier part of the devices is smaller and less traumatic.
2. Non-medicated IUD: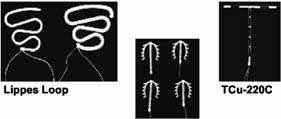
No drugs are added to the matrix or plate form of the IUD. It consists of plastic polyethylene and copper. There are so many types of this group. The most commonly used are copper T, TCU 380A, Multiload 375 and Nova T.
Newer developments aim to reduce side effects and decrease expulsion rate by producing smaller and  lighter IUDs.
lighter IUDs. 
MECHANISM OF ACTION OF IUDs
1. Prevent implantation of the fertilized oocyte
2. Produce a local sterile inflammatory reaction in the endometrium as a result of the presence of a foreign body causing spermicidal effect, and the presence of copper increases this reaction and also increases the local release of prostaglandins thus decreasing the rate of pregnancy.
3. They diminish sperm transport through the cervix to the oviduct by increasing the thickness of the cervical mucus (this happens with the hormonal IUD).

4. Steroid-releasing devices induce progestational changes that result in endometrial gland atrophy& Inhibit further development of the ova.
TIME OF INSERTION OF Intra-uterine contraceptive device
The best time to insert IUD is during the menstrual cycle at any day of the week following menstruation, which indicates that the woman is not pregnant.
After delivery either vaginally or by caesarian section; an eight-week delay seems to be adequate. IUDs specifically designed for immediate post partum insertion are now available.
-Following spontaneous or therapeutic abortion, an IUD can be inserted immediately, but the risk of expulsion is increased in the second-trimester abortion.
REMOVAL OF Intra uterine contraceptive devices
IUD should be removed only in the late luteal phase of the cycle or the first seven days of the cycle, unless pregnancy is desired.
If the woman reaches menopause, the IUD should be left in situ for one year after the last menstrual cycle.
- IUD should be removed if the thread is not visible.Removal is done by a specially designed hook or a pair of artery forceps, preferably under ultra sound guidance.
UNDESIRABLE EFFECTS OF IUD
1. MENSTRUAL DISTURBANCES:
This includes both regularity and excessive blood loss, i.e. menstrual cycles become prolonged and heavier (menorrhagia) and also may cause dysmenorrhea.
But-levenorgestril releasing IUDs decrease the monthly blood loss.
 IUD Penetrating the
IUD Penetrating thewall of the uterus
2. PERFORATION
This can occur at the time of insertion.The incidence is 1.3 of every 1000 cases. It may be best prevented by straightening the uterine axis through pulling the tenaculum which holds the cervix and by performing a bimanual examination to check if the uterus is anteverted or retroverted before attempting to insert the IUD.
3. EXPULSION OF Intra-uterine contraceptive device
Rate of expulsion varies from 1_7/100 women in first year of use. Expulsion is commoner in the first three months of use so that every woman should be examined frequently and should be taught to feel the thread of the IUD vaginally frequently.
4. PELVIC INFECTION
This is caused by bacteria carried into the uterus at the time of insertion. But having the pelvic inflammatory disease after insertion usually results from sexually transmitted bacteria . The consequences of these bacterial infections in the ovaries it may cause salpingitis, tubo- ovarian abscess, or pelvic peritonitis and tubal blockage. Symptomatic pelvic inflammatory disease is frequently treated with antibiotics without removing the IUD until the symptoms resolve, then a new IUD should be inserted under aseptic technique.
5. PREGNANCY ON TOP OF IUD
 Pregnancy with IUD
Pregnancy with IUDThis doesn't happen unless the IUD is not in its proper place in the endometrial cavity (slightly low or tilted) so an intra uterine pregnancy may ensue.
ECTOPIC PREGNANCY
IUD prevents intrauterine pregnancy but not ectopic pregnancy, so the relative incidence of ectopic could be higher in IUD users.
SPONTANEOUS ABORTION
A spontaneous abortion rate of up to 55% has been reported in women becoming pregnant on top of IUD, which is not removed after being pregnant. However, if the IUD appendage is visible it, should be removed or it might be expelled without any intervention, abortion rate diminished after that. If the thread is not seen, it is not advisable to perform uterine probing because of increased risk of perforation, abortion, and/or sepsis.
PREMATURITY
Reported cases of preterm deliveries have been found in patients with an IUD in situ.
EFFICACY OF Intra-uterine contraceptive devices
Throughout the years, pregnancy rate among IUD users has decreased steadily. Non medicated IUDs and copper IUDs (up to 200) had up to 3% pregnancy rates.
CONTRA-INDICATIONS FOR THE USE OF IUD
RELATIVE CONTRAINDICATIONS of Intra uterine contraceptive devices
1. Nulliparity
2. Valvular heart disease and cardiomyopathy
3. Previous ectopic pregnancy
4. Moderate to severe anemia
5. Hypermenorrhea or menorrhagia
6. Wilson's liver disease
7. Copper allergy
8. AIDS
9. High risk of STD
ABSOLUTE CONTRAINDICATIONS of Intra uterine contraceptive devices
1.Cardiomyopathy
2.Recent acute pelvic inflammatory disease
3.Chronic or recurrent PID
4.Recent septic abortion
5.Acute cervical or vaginal infection
6.Congenital uterine anomalies
7.Uterine tumors
8.Undiagnosed uterine bleeding
For whom Intrauterine Contraception is appropriate
Women of any reproductive age willing for long-term, highly effective contraceptive
CONCLUSION
The benefit of IUD use surpasses its risks, and these are the risks of pregnancy on top of IUD. IUDs are strongly advised for most women seeking contraception in developing countries because it has the highest continuation rate and the lowest cost…….
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
