Female genital tract
It is formed from external and internal organs:
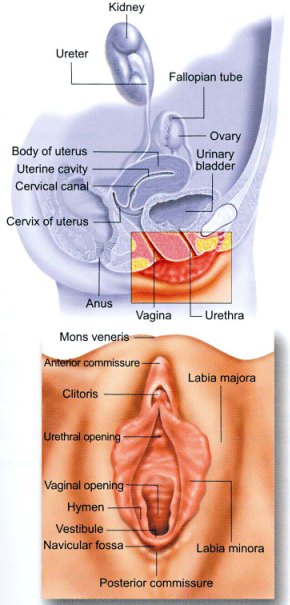
A-External female genital organs:
It is formed of organs around the vaginal opening:
-Pubis:
It is the groin folds covered with hair, in mature adult woman it is horizontal in shape, it is not present in childhood, and it gets smaller after menopause. Hair growth at this area is one of the signs for puberty.
-Labia majora.
-Labia minora.
-Clitoris:
It is equivalent to the penis in the male external genital organs, it about 2.5cm (1inch) in length and it is formed from tissues that are highly supplied with blood vessels that gets congested during orgasm at the time of intercourse.
-Hymen:
It has different shapes, usually its incomplete membrane with an opening that allows blood to come out through this opening, it could be torn during the first intercourse, but hymnal remnant may remain after several times of intercourse.
-Bartholin’s gland:
It lies at both sides of the vagina, and its function is to secret mucosal secretions that help in lubrication during intercourse.
-Urethral orifice:
It lies just below clitoris.
 Genital Area Hygiene
Genital Area Hygiene
B-Internal Female Genital Organs:
-Vagina:
It starts from the hymen till the cervix, it is lined with folded skin, and it’s around 10cm in length, but it is stretchable and becomes longer during labor and intercourse.
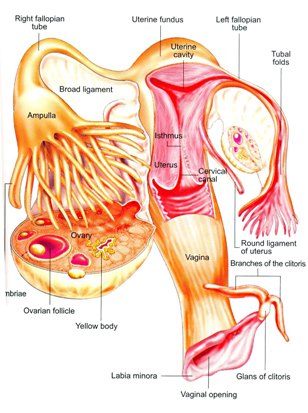
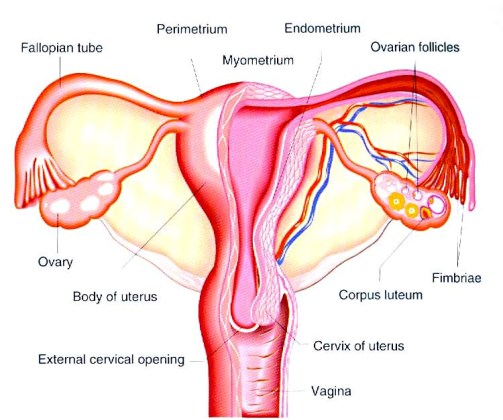
-Uterus:
It’s like an inverted pear in shape, 7.5cm in length, 5cm in width, it starts from the cervix then uterine body and it’s lined by endometrium which is a special layer that lines the inside of the uterus, and gets thickened before each cycle in response to hormonal changes, then sheds out with cycle in the form of menstrual blood followed by formation of a new layer.
-Fallopian tubes:
Extend from uterine body to the ovary with an average length of 11cm, and ends with a finger like processes, it is lined with certain type of cells that helps in transporting the oocyte from the ovary to the uterus, fallopian tubes are the sites where fertilization and the early stages of fetal development happen.
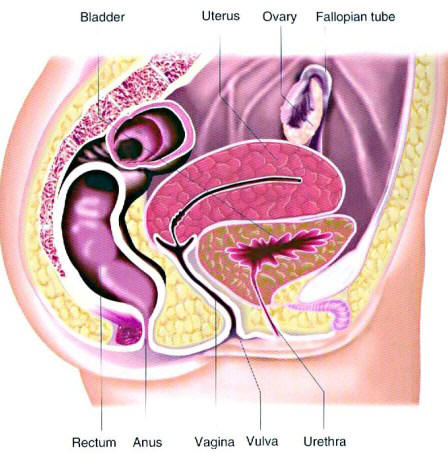
Cross Section of Female Pelvis
Video of Female Reproductive System
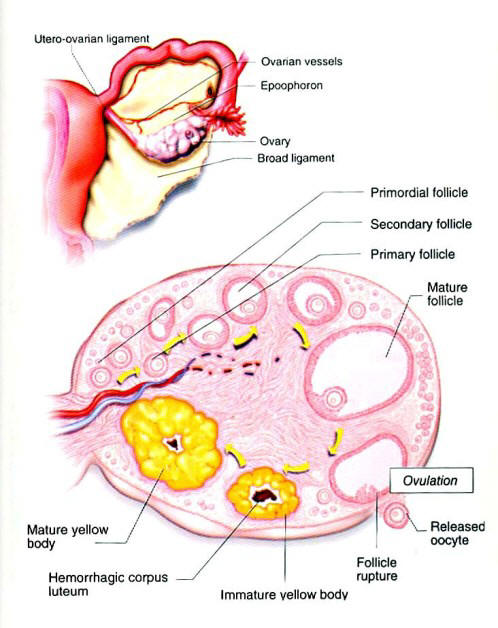
-Ovary:
There are two ovaries at both sides of fallopian tubes they are formed from the external layer (cortex) that contain the follicles and inner layer (medulla) in between there are blood vessels and nerves, ovaries are equivalent to testis in the male, ovaries produce two hormones estrogen and progesterone .
Internal female genital organs
We will try to explain simply and as clear as we could what is the regular monthly cycle and what are the physiological changes that happen during each cycle, several hormones from different body organs control menstruation.
The most important of which are:
-At the base of the brain there is a gland called hypothalamus which secrets GNRH hormone.
-Just beneath the hypothalamus there is the pituitary gland that secrets two hormones FSH and LH, their secretion is under the effect of GNRH hormone.
-LH and FSH have a direct effect on the ovary to stimulate follicular growth and maturation, eventually ovulation at middle cycle and one oocyte is ready to be fertilized. The fertilized oocyte passes through fallopian tube to reach the endometrium, where the fetus grows, so if any blockage in one or both of fallopian tubes will affect pregnancy rate and any disturbance or decrease in the secretion of any previous hormone will affect fertilization.
Let’s explain it in details:
The hypothalamus starts secreting GNRH hormone in a pulsatile manner; this will induce the pituitary gland to secrete FSH and LH hormone, so its secretions differ during different stages of the cycle. During the first half of the cycle (before ovulation) GNRH is secreted every 1-1.5 hour, but after ovulation it is secreted much less frequent (every 4 hours).
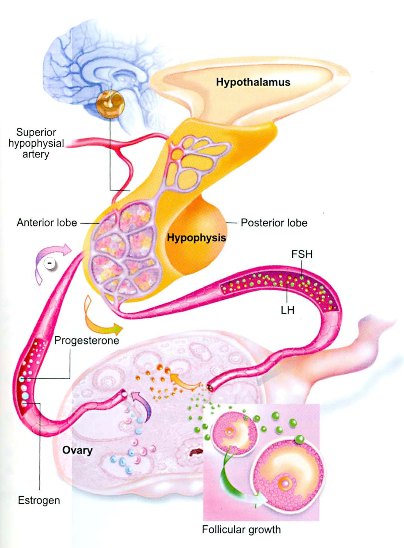
Glandular Control of Menstrual Cycle
During the first half of the cycle there are low levels of estrogen, this will stimulate GNRH secretion which will stimulate the pituitary gland to secret FSH and LH hormones, these hormones induce the ovary to start follicular production, when the oocyte forms it starts to secrete estrogen hormone so its level in blood will start to increase gradually during this time one of the follicles will be mature more than the other follicles and will grow faster and secret larger amounts of estrogen, rising level of estrogen causes a decrease in FSH and LH secretion, since the dominant follicle is capable of rapid growth, and fertilization it continue to grow despite high FSH level.
Rising level of estrogen helps in more maturation of the follicle, and in building up the endometrium. Estrogen level continues to increase until it causes a sudden increase in LH level, which is important in the final maturation of the follicle. 36 hours after this sudden increase ovulation happens during normal cycle, LH increase at day 12 of cycle and ovulation at day 14, after ovulation the oocyte is released, the follicle shrink to form the corpus luteum at outer layer of the ovary and it continue to secret estrogen and progesterone.
Menstrual cycle:
Both estrogen and progesterone decrease pituitary gland secretion of FSH and LH. If there is fertilization corpus luteum continue to secret estrogen and progesterone to prepare the endometrium to be ready for the fertilized ovum, after the third month of pregnancy the placenta forms and start to secret estrogen and progesterone and corpus luteum disappears.
If there is no fertilization (or pregnancy), corpus luteum disappears and shrink gradually 10 days after ovulation which result in drop in the level of estrogen and progesterone, two weeks later the endometrium sheds out in the form of menstrual bleeding, and the drop in hormonal level result in increase in GNRH, and initiation of new cycle.
It should be mentioned here that each follicle is formed from the oocyte surrounded by fluid, at the first half of cycle it is small in size, but at time of ovulation it reaches 16-26mm; this increase in size is due to increase in amount of fluid around the oocyte, (this increase in size can be followed using ultrasound), 36 hour before ovulation it grows faster, once LH level increase, ovulation happens. Regarding endometrial changes; at the first half of cycle (proliferative phase) when estrogen level is high, the endometrium increase in thickness and in blood supply, and then the endometrial glands start to secret mucosal substances that nourish the endometrium to be ready for the fertilized ovum this phase is called secretory phase if there is no pregnancy, the corpus luteum dissolves, estrogen and progesterone level decrease which leads to shedding of the endometrium and menstruation.
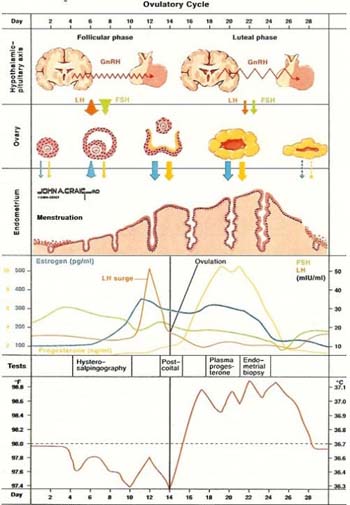
Ovulatory Cycle
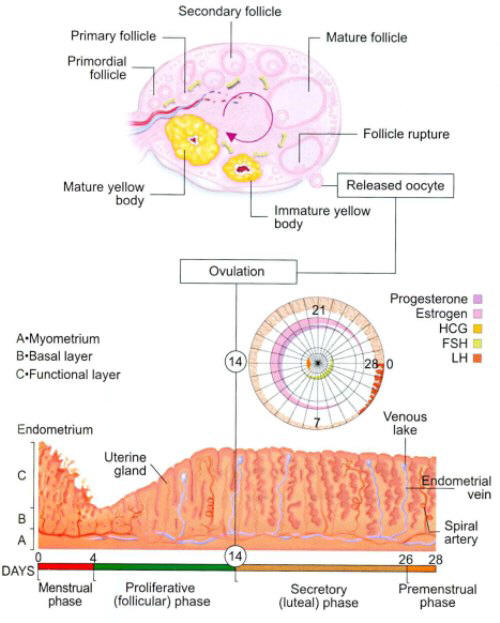
Ovulatory and Endometrial changes during the Menstrual Cycle
Dear readers:
You may have some questions that cross your minds, we are glade to answer what we think is important for you?
How many oocytes does the woman have at birth?
At birth both ovaries contain around 2million oocyte; these remain dormant till puberty and most of them would have atresia, that is why at puberty their number decrease to 400.000 oocyte, the process of atresia continue, it is a lifelong process even during pregnancy, during each menstrual cycle about 20 follicle starts to grow, but only one follicle reaches maturation, and the rest of them disappear.
There are many factors that affect the rate of atresia, some are genetic and hereditary factors, but some are related to the environment like irradiation, medication, and smoking; that’s why the age of menopause (the age when menstruation stops) differs from one woman to another, that’s when all the oocytes go into atresia.
What is the follicle?
It is some sort of a sac filled with fluid that contains the oocyte inside.
How does ovulation happen? How could the oocyte come out of the follicle?
LH hormone is secreted from the pituitary gland; when the level of this hormone increase, it leads to formation of something like a hole in the membrane of the follicle, the oocyte comes out to be catch by the fimbrial end of the fallopian tube (finger like processes mentioned before).
Stages Of Oocyte Maturation
Does ovulation happen in alternating manner between each ovary?
Not exactly like that, ovulation whether from the right or left ovary is a random process, and you can never know which ovary will have the ovulation from till one or two days prior to ovulation and that can be done using ultrasound.
This question is so important for women with only one fallopian tube, most of the time the tube catches the oocyte from the ipsilateral ovary, but there are reported cases of pregnancy in women with one tube (on the left for example) and one ovary on the other side (on the right side) which is an indirect evidence that the fallopian tube can catch the oocyte from the contralateral ovary.
What is the regular menstrual cycle?
It is the cycle that its duration is between 26-34 day starting from the first day cycle till the first day of the next one, and lasts from 3 to 5 days with average bleeding.
Does having a regular cycle means necessarily that ovulation happened?
Usually yes, but there are some exceptions in which the follicle grows incompletely, but still has the capability to secrete the hormones necessary for endometrial changes and menstruation.
Generally irregular cycles mean that most likely there is no ovulation.
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
